
Confirmation bias in decision making is largely unintentional and often results in ignoring some information. Existing beliefs can include one’s expectations in a given situation and predictions about a particular outcome.
People are especially likely to process information to support their own beliefs when the issue is highly important or self-relevant.
When we see a young person in school or the community and they are having challenges with learning impacting on their behaviour, we can draw conclusions which may come from a limited set of information. How we view the young person may also be influenced by training and experiences that we have had.
Time pressures and a lack of knowledge have also been cited by teachers as factors which negatively influence the ability to support pupils for example with ADHD.1 In one study where referrals of ‘Children in Care’ and adopted children were referred to a specialist Child and Adolescent Mental Health Service (CAMHS) team , they found under-diagnosis of common Neuro developmental Disorders (NDDs) and mental health conditions but over-diagnosis of attachment disorder.2
There had been an assumption, because they were in care, that their challenges were all related to attachment and Neurodevelopmental Disorders had been overlooked.
Checking out our assumptions
Having the ability and opportunity to gather information allows us to consider the different potential conclusions.
Let’s start by looking at Jack. He was born in April 2007. Read the following box and write some notes about your initial thoughts about Jack and his challenges. At this point you only have this information.

What did you think?
In reality these are two children born on the same day but in two very different places by two sets of very different parents in the UK . Jacob is from Marlow and Jack from Middlesbrough. When you start comparing the two boys you start to see the same presenting challenges in school but potentially very different interpretations.
Additionally, there are huge differences in their lives.
| Jacob A | Jack B | |
| Parental qualifications | Both graduates. | No higher qualifications than 3 GCSES or below. |
| Parents | Mum dyslexic. At home with one other child. Dad working in well paid job. He has good mathematical and IT skills. | Mother depressed, drinks excess alcohol and has been the victim of domestic violence. One other younger child. Dad in and out of prison for dealing drugs. Dad has good mathematical skills. |
| Family History | Many family members (and extended family) have a diagnosis or symptoms of signs of Developmental Coordination Disorder, Dyslexia, ADHD and Autism. | Depression, Anxiety, Substance misuse. |
| Child in Care | No | Several times. |
| Nutrition | Well balanced meals. Fresh fruit and vegetable every day including a ‘Smoothie at breakfast’. Omega 3 and multi-vitamin supplementation each day. | Often misses breakfast. Only likes one type of sweetened cereal. No fish in diet. Mainly brown and processed food. Fruit once or twice a week. On Free School Meals. |
| Home | 2 computers, 2 I-Pads, 2 TVs, 2 smart phones. Garden has climbing frame, and football goal. 100+ books of all types. Parents read every day with Jack, Lego, creative play, plays Minecraft. Lots of craft activities at home. Eats at the meal table every day. | 1 TV and 1 Pay -as- you- go Smartphone. School book only at home. Mum has difficulties reading and spelling. Child loves playing on cousin’s computer on Minecraft. No table to eat at. |
| School | School has forest school, is a Microsoft Academy, and won an award for nutritious school meals. | Inner city school on Special Measures. 50% of children have been excluded at one point.3 |
| EHCP | Has a diagnosis of Autism, Developmental Language Disorder, Developmental Coordination Disorder(DCD), and Attention Deficit Hyperactivity Disorder. | Has a diagnosis of SEMH (Social and Emotional and Mental Health) Been excluded twice. On 3 year waiting list for ADHD assessment . |
| Jack in class | Top in the school in a computer Maths game. Has TA support one- to- one for 20 hours per week. Has SALT, and OT support. | Difficulties with reading. Been in specialist unit for ‘SEMH’ because of disruptive behaviour. No SALT. EP monitoring. |
Jacob and Jack live very different lives there is no doubt. However, their challenges presented in school are the same but the interpretation has been different resulting in different outcomes. Their lives differ in so many ways that can impact on their learning outcomes. This includes the daily patterns and habits such as the opportunity to read and have conversation, a table to sit at and nutritious food to eat, outdoor space to play and computer access to play and learn.
Jack’s Mum has had to survive on very little money, with her partner in and out of prison. There is an example of intergenerational impact. Jack’s mum left school at 16 years with no qualifications and low literacy skills. She is concerned for Jack, but doesn’t know how to access help or what there is. She has no internet access apart from her phone and low digital skills. She is, not surprisingly, depressed and because of her poor self-care Jack has gone into foster care for periods of time in the last couple of years.
Jack’s father is one of the one-in-three in prison7 who has also undiagnosed ADHD and long- term dependency on a variety of illegal substances. His impulsive behaviour and addictive nature has got him into trouble. If you met him you would say he was bright and articulate but gets frustrated and has hit Jack’s mother a number of times.
In school Jack gets frustrated in class as he doesn’t always understand what is being asked of him. This results in him being disruptive. His social skills are poor and his speech is not always clear. His reading and writing is falling further behind during this last year. He has few friends and intermittent schooling has made him even more isolated.
Jacob’s life is very different. He has educated parents whose nursery alerted them to Jacob’s speech and language delay. They sought information and were able to navigate the system and gained an early and comprehensive diagnosis for Jacob.
They have got professional help for him. He is at a primary school with a forest school and with an impressive computer access.
He has an Educational Health Care Plan. He has time allocated with a teaching assistant who helps him navigate times of change in class and keeps him on task and reinforcing positive social interactions that he has difficulty with.
Without this help Jacob can be very disruptive to others in class. During Covid-19 he has gone into school for some of the sessions and been using the computer even more at home and learned to code. He has also become top in his school for an online maths game. This has changed the school’s perception of him and can see he has some real talents in mathematics and IT.
Different balls in the bucket?
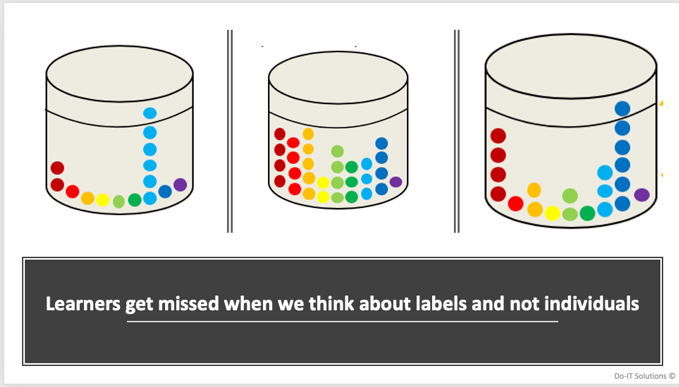
If we use an analogy of balls in the bucket which represent different strengths and challenges in the young person’s life we sometimes only view balls of a certain colour. We give a diagnosis only when a threshold is reached. Taking a dichotomous approach rather than starting with a needs assessment means that some children miss out on support as they are not ‘bad enough’.
Creating a young person’s profile
Each child will have an individual profile of needs and abilities. There will be different local and social factors that result in different pathways to diagnosis (or not). Intersecting and compounding forms of discrimination and disadvantage create these different outcomes.
Remember Jack and Jacob have the same profile of challenges but the ‘wrap around’ in their lives is significantly different. One child has an EHCP for neurodevelopmental conditions and the other a label of SEMH. We can see poverty at play in Jack’s life. Middlesbrough has four times the level of Free School Meals compared to Marlow.6
Socio-economic status is linked to longer term outcomes and increasing impact as children progress. It also relates to parental resources, the locality of the school and quality of teaching and a disconnect between home and school.8
What is SEMH?
Social, emotional and mental health (SEMH) needs has been defined as a type of special educational needs in which children/young people have severe challenges in managing their emotions and behaviour. They often show inappropriate responses and feelings to situations.
Some characteristics of children with SEMH may include:-
- Disruptive, antisocial and uncooperative behaviour
- Temper tantrums
- Frustration, anger and verbal and physical threats / aggression
- Withdrawn and depressed attitudes
- Anxiety and self-harm
- Stealing
- Truancy
- Substance misuse
Have Jack’s challenges been viewed as ‘behaviours’ and assumed to be more associated with the external factors than potentially related to neurodiversity as well ?
Children born in Middlesbrough are more likely to be absent from school than national and regional averages and more likely to be excluded from school. Fourty percent of children who are in local authority care have Special Educational Needs (SEN), 20% have an Education, Health and Care Plan.
If we miss vital information we can end up drawing the wrong conclusions. Interestingly, when we look at data from children who have an Education, Health Care Plan and compare those in care from the mainstream population we can see significant differences in their diagnosis.4,5
| Children in care with EHCP4 | All children | |
| Diagnosis of Autism Spectrum Disorder | 12% | 29% |
| SEMH | 40% | 12% |
| Speech, Language, Communication challenges | 9% | 15% |
Why should it be that Jack is more likely to get a diagnosis of SEMH rather than Autism or Speech Language and communication challenges ?There is good evidence of higher rates of neurodiversity among children excluded from school like Jack but usually no routine screening for these traits.
In one study of excluded children the rate of ASD was 20 x the national average9. In the large- scale longitudinal study in Avon ALSPAC cohort of those excluded by age 8 years, 19% had ADHD and 23% had language development in bottom 10%.10
In an older study a sample of pupils who had been permanently excluded pupils from thirty-three Sheffield secondary schools found that 76% were ≥2 years behind their peers in reading.11 Despite extensive evidence of co-occurrence between conditions and this also interlinked with adversity we often still seek single diagnoses for children who have intersecting challenges.12
Considering neurodiversity as a concept
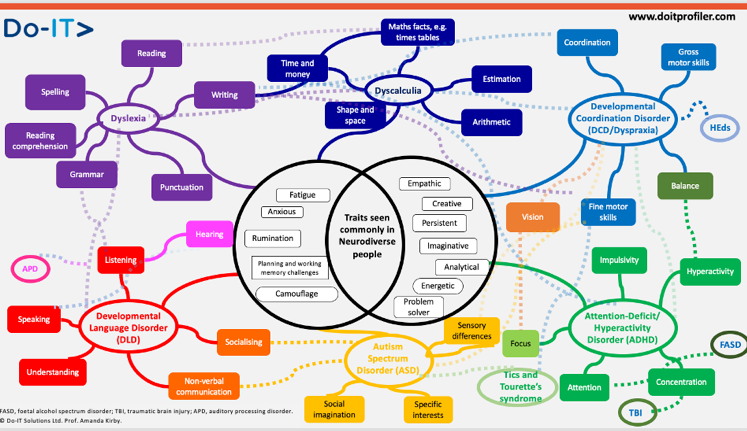
Note: FASD, Foetal Alcohol Spectrum Disorder; TBI, Traumatic Brain Injury; APD, Auditory Processing Disorder.
A picture of neurodiversity
This term recognises the fact that our brains (neuro-) naturally vary from person to person (are diverse) and are a part of human variation. It takes a dimensional approach rather than a categorical one. It was coined by Australian Sociologist Judy Singer in the late 1990s.
By embracing the concept of neurodiversity and recognising the extensive evidence of co-occurrence it allows us to move from a narrow diagnostic approach to a whole-child needs approach. We can create a formulation from information gathered from multiple sources and support children functionally.
This allows each child to potentially have equal opportunity to gain support earlier and reduce biases. If we continue to have a model that only intervenes with a diagnosis Jack will become an unemployed Dad and the cycle will continue.
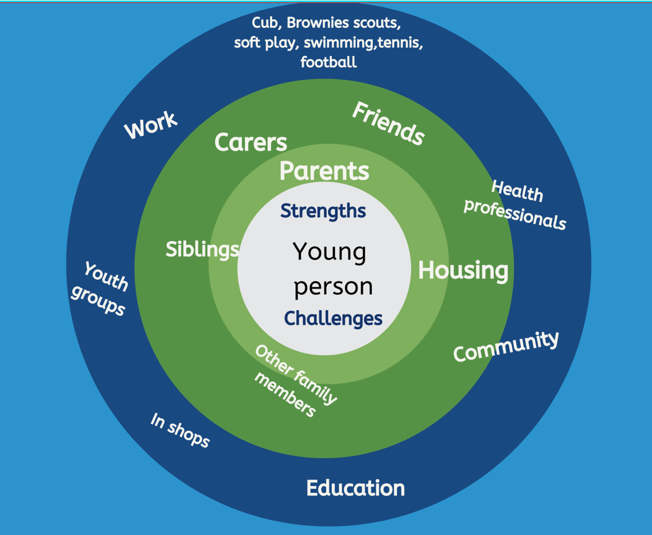
A whole child approach is a systemic approach considering the child in the context of their lives and the society they live in but is not judgemental. Bronfenbrenner 13, was one of the first people to discuss the need to understand the ecology of the child.
The cost for families and to society
Jack’s mum doesn’t have access to the internet apart from her pay-as-you- go phone and if she did, she wouldn’t know where to ask for information or be able to read or complete forms she would need to fill in ( I checked one site for a local authority and the website had no accessibility tools and needed a reading age of someone in Year 12 to understand and read the content!)
Jacob is at a great school and getting support but without help he would have no friends, his behaviour would easily spiral and he could also be a statistic as a child moved to alternative provision. So often children developed secondary challenges as a consequence of the delay or misdiagnosis.
We need to see ‘behaviour’ as a means of communication and never a diagnosis. Increasing the ability for early identification can also reduce the flow downstream and for some stop the route into the justice system. The economic impact for society is great. Inclusion is all about equity and reducing the disparities in society to allow both Jack and Jacob to have a chance of a bright future.
Building a picture of the 6 Ps
- Pre and in service training across neurodevelopmental disorders
- Precipitating challenges now
- Perspectives i.e., context e.g., home, school
- Predisposition to increased risk of ‘fall out’ from past and present events e.g., ACEs, illness, loss, LACYP, trauma and head injury.
- Protective factors e.g., scaffolds in place, parental support, intervention, improved nutrition.
- Positive factors e.g., strengths, resilience, self-esteem, peers.
Professor Amanda Kirby is CEO of Do-IT Solutions. Until recently she held a chair in developmental disorders at the University of South Wales. She is a qualified GP and worked for some years in adult psychiatry.
References:
1.Woolgar M & Baldock E (2015). Attachment disorder versus more common problems in looked after and adopted children: Comparing community and expert assessments. Child & Adolescent Mental Health. 20(1), 34-40.
2. Richardson, M. Moore, D. Gwernan-Jones, R. Thompson-Coon, J. Ukoumumme, O. Rogers, M. Whear. R. Newlove-Delgado T. Logan, S. Morris, C. Taylor, E. Cooper, P. Stein, K. Garside, R & Ford, T. (2015). Non-Pharmacological Interventions for attention-deficit/hyperactivity disorder (ADHD) delivered in school settings: systematic reviews of quantitative and qualitative research. Health Technology Assessment. 19 (45) 1-470.
3. https://www.gazettelive.co.uk/news/teesside-news/children-deserve-better-dozens-school-19261462 ( Accessed March 2nd , 2021)
4. https://explore-education-statistics.service.gov.uk/find-statistics/characteristics-of-children-in-need/2020 ( Accessed March 2nd , 2021)
5. Children Looked After in England (2019) https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/850306/Children_looked_after_in_England_2019_Text.pdf
6. https://lginform.local.gov.uk/reports/lgastandard?mod-metric=2174&mod-period=1&mod-area=E10000002&mod-group=AllGeographicalNeighbours&mod-type=comparisonGroupType ( Accessed March 2nd , 2021)
7. Young, S., Gudjonsson, G., Chitsabesan, P. et al. Identification and treatment of offenders with attention-deficit/hyperactivity disorder in the prison population: a practical approach based upon expert consensus. BMC Psychiatry 18, 281 (2018). https://doi.org/10.1186/s12888-018-1858-9.
8. Socioeconomic Disadvantage, School Attendance, and Early Cognitive Development: The Differential Effects of School Exposure. Ready, Douglas D. Sociology of Education, 2010, Vol.83(4), p.271-286
9. Barnard, J., Prior, A. & Potter, D. (2000)Inclusion and autism: is it working?
10. Paget, A. et al.(2018) Which children and young people are excluded from school?
Findings from a large British birth cohort study, the Avon Longitudinal Study of Parents and Children (ALSPAC). Child. Care. Health Dev. 44, 285–296 (2018).
11. Galloway, D., Martin, R. & Wilcox, B. Persistent Absence from School and Exclusion from School: the predictive power of school and community variables. Br. Educ. Res. J. 11, 51–61 (1985).
12.Cleaton MAM, Kirby A (2018) Why Do We Find it so Hard to Calculate the Burden of Neurodevelopmental Disorders? J Child Dev Disord. 4:10.
13. Bronfenbrenner U. The ecology of human development. Cambridge: Harvard University Press; 1979.
Register for free
No Credit Card required
- Register for free
- Free TeachingTimes Report every month